Why we should all wear masks
Abril 2020
Covid -19 : Why we should all wear masks — There is new scientific rational
Written by Sui Huang Institute for systems Biology
The official recommendation in the United States (and other Western countries) that the public should not wear face masks was motivated by the need to save respirator masks for health care workers. There is no scientific support for the statement that masks worn by non-professionals are “not effective”. In contrary, in view of the stated goal to “flatten the curve”, any additional, however partial reduction of transmission would be welcome — even that afforded by the simple surgical masks or home-made (DIY) masks (which would not exacerbate the supply problem). The latest biological findings on SARS-Cov-2 viral entry into human tissue and sneeze/cough-droplet ballistics suggest that the major transmission mechanism is not via the fine aerosols but large droplets, and thus, warrant the wearing of surgical masks by everyone.
The surgeon general tweeted: “STOP BUYING MASK, they are not effective…”. The Center for Disease Controls (CDC) states that surgical masks offer far less protection than the N95 respirator masks (which also must be perfectly fitted and only professionals can do it). The CDC recommends that healthy persons should not wear masks at all, only the sick ones. These guidelines are not rooted in scientific rationales but were motivated by the need to save the valuable masks for health professionals in view of a shortage. But they may have had unintended consequences: stigmatizing those that wear masks in the public (you are a hoarder, or you are contagious!)
Contrast this with the cultural habit, the encouragement, or even mandate to wear masks in Asian countries — which have now “flattened the curve” or even have had a flatter curve from the beginning.
Sure, surgical masks, and improperly worn N95 respirator masks, do not offer perfect protection. But if the stated goal is to “flatten” the curve (as opposed to eradication of the virus), we have to abandon the black-and-white thinking, and embrace shades of grey. We cannot any longer claim that masks “are not effective”. We cannot allow the perfect to be the enemy of the good. What if a however partial protection afforded by leaky surgical or even self-made masks reduces transmission probability to an extent that is similar to that of the recommended (equally imperfect) distancing by more than 6 feet from each other or “not touching your face”? It could then double the impact of non-pharmacological intervention (NPI) on flattening the curve (FIG. 1).
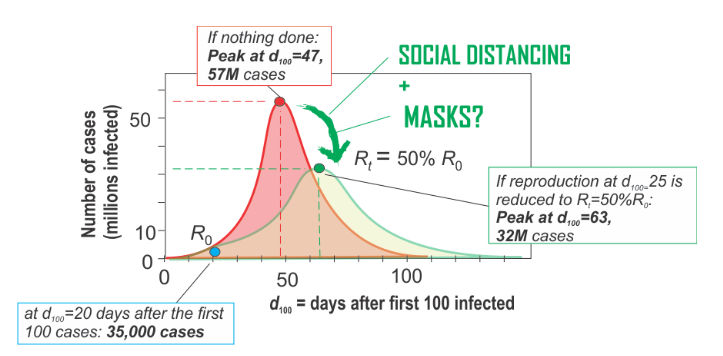
Figure 1. “Flattening the curve”. Effect of mitigating interventions that would decrease the initial reproduction rate R0 by 50% when implemented at day 25. Red curve is the course of numbers of infected individuals (”case”) without intervention. Green curve reflects the changed (”flattened”) curve after intervention. Day 0 (March 3, 2020) is the time at which 100 cases of infections were confirmed (d100 = 0).
The model is only for illustration and was performed in the SEIR-model simulator (http://gabgoh.github.io/COVID/index.html). The non-intervention model was fitted to these data points: a time period of twenty days in which the number of cases in the United States has risen from 100 (d100=0) to 35,000 (d100=20). Standard parameters were used (population size 330 M, Tinc=5.2 days, Tinf = 3.0 days but with the rather high value R0=5.6 in order to achieve the observed rate of increase of case numbers in the U.S. The curves are redrawn not to scale.
Since the CDC provides no scientific evidence for its statement that masks worn by the public “are not effective”, here we review the scientific support for protection conferred by surgical masks. We focus on mechanistic rationale (as opposed to epidemiological-phenomenological evidence). We conclude, by considering cough droplet ballistics and the latest research findings on the biology of transmission of the SARS-CoV2 virus (which causes COVID-19) that any physical barrier, as provided even by make-shift masks, may substantially reduce the spread of COVID 19. If we are soon to yield to the pressure to loosen lockdowns and allow limited social interactions to revive the economy, then public masks should have a role and could facilitate a middle-of-the-road approach.
The official recommendation by CDC, FDA and others that masks worn by the non-health-care professionals are ineffective is incorrect at three levels: In the logic, in the mechanics of transmission, and in the biology of viral entry.
I. THE LOGIC
Of course no mask, be it the tight-fitting NIOSH approved N95 respirator mask or the loosely worn surgical mask, provide perfect (“100%”) protection. But imperfect protection does not mean “completely useless”, much as a glass not full need not be empty: I would gladly accept a glass of water filled to 60 % when I am thirsty. Absence of evidence (of protection) is not evidence of absence. But in our binary world, the official message that surgical masks are “not effective” may have sent the wrong message: that they are absolutely useless. Sadly, with the black-and-white picture painted by officials, the discussion about the effectiveness of masks has been stifled, and with it the possibility of incentivizing industry to ramp up production of these 75 cents-a-piece protective devices.
But with the declared goal to “flatten the curve” (and not to totally eliminate the virus) we have a “relative” as opposed to absolute goal, which places the notion of “partial protection” in a new light. In principle, one could compute the extent Y of flattening of the curve given a partial protection by X % as conferred by mask. But for that we need to first understand the mechanics and biology of transmission in detail.
II. THE MECHANICS
How viruses that cause airborne diseases are carried by droplets from person to person is a complicated, understudied matter. Droplets can (for this discussion) be crudely divided in two large categories based on size (FIG. 2):
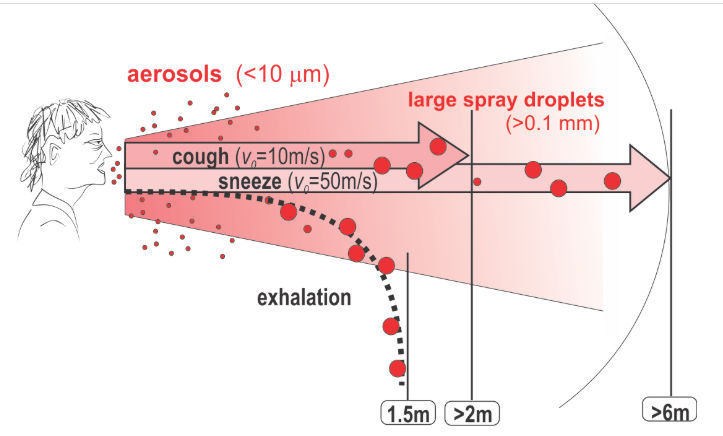
Figure 2.
Droplet larger than aerosols, when exhaled (at velocity of <1m/s), evaporate or fall to the ground less than 1.5 m away. When expelled at high velocity through coughing or sneezing, especially larger droplets (> 0.1 mm), can be carried by the jet more than 2m or 6m, respectively, away.
(a) Droplets below a diameter of 10 um (micrometer), the upper size limit for the definition of ‘aerosol’ (particles so light as to be able to float in the air). For brevity, let us call this category “aerosols”. These small aerosols are carried by ventilation or by winds and thus can travel across rooms. What makes N95 facial masks different from the surgical masks is that the former are designed (as per regulatory requirement) to stop aerosols: they have to filter out 95% of droplets smaller than 0.3 um.
(b) Droplets larger than 10um (micrometer), reaching 100um (0.1mm) or more. Let us call these large particles “spray droplets” here. (For a more detailed discussion, see Nicas and Jones, 2009). Of course, droplets can be even larger, up to a size visible to the naked eye in the spray generated by coughing or sneezing (0.1 mm diameter to above). Calculations by Xie et al suggest that if exhaled, the >0.1 mm droplets may evaporate or fall to a surface within 2m, depending on size, air humidity and temperature.
But coughing or sneezing can shoot them like projectiles out of the mouth with a “muzzle velocity” of 50 meters/second (for sneezing) or 10 m/s (for coughing), and droplets can reach distances as far as 6m away. If so, then the much mentioned “safe distance” of 6 feet in social encounters may not suffice — except you wear a (simple) mask –more on that later.
Here is the central biological implication of the distinction between aerosols and spray droplets: For airborne particles to be inspired and reach deep into the lung, through all the air ducts down to the alveolar cells where gas-exchange takes place, it has to be small (FIG. 3): only droplets below 10 micrometer diameter can reach the alveolae. By contrast, the large spray droplets get stuck in the nose and throat (the naso-pharyngeal space) and in the upper air ducts of the lung, trachea and large bronchia. The droplets of a typical cough expulsion have a size distribution such that approximately half of the droplet are in the categories of aerosols, albeit they collectively represent only less than 1/100,000 of the expelled volume (Nicas et al 2005).
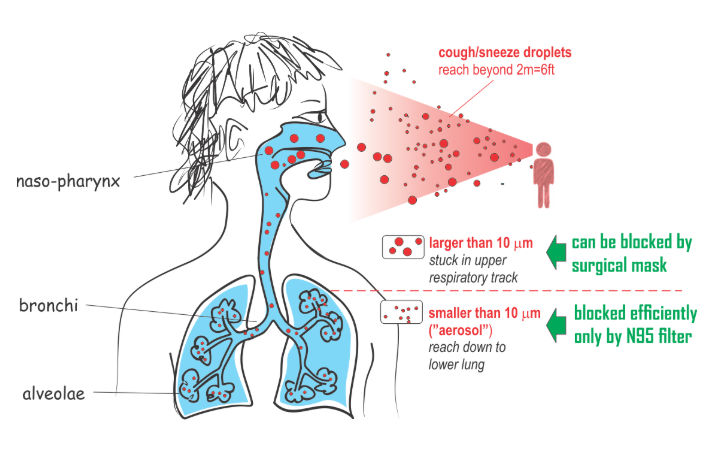
FIGURE 3. Anatomy of airways and where droplets can end up, depending to their size and what droplets are blocked by what masks
It thus follows that the sophisticated N95 masks, designed to filter out the smallest particles, help to prevent droplets from carrying the virus down to the alveolae. But is this really relevant for flattening the curve? We shall see below. By contrast, it is plausible that the large droplets that end up in the nasopharynx can be stopped by any physical barrier, such as simpler surgical or dust masks.
Of course many aerosol droplets in the exhalation or cough spray may not contain the virus, but some will do. In the case of the SARS-Cov-2 virus it is not known what the minimal infectious load is (number of viral particles needed to start the pathogenesis cascade that causes a clinical disease). But we begin to appreciate whether the small aerosol or large projectile droplets are more relevant.
The tacit notion at the CDC that the alveolae
are the destination site for droplets to
deliver the virus load (the alveolae are after all the anatomical
site of life-threatening pneumonia), has elevated the apparent
importance of N95 masks and led to the dismissal of surgical masks.
Nuances do not translate to the lay people (as well as many arm
chair experts) who now, owing to message binarization, think that
masks are useless.
Even with respect to the small aerosols we must not forget that the partial
filtering provided by surgical masks is better than nothing. In an experimental
simulation of the filtering capacity of masks in 2008,

FIGURE 4
What the authors found for inward protection warrants some
questioning of CDC’s message that surgical masks are “not effective”:
While FFP2 (or N95) masks indeed filtered out >99% of particles (thus,
reducing the aerosol load by 100-fold), the surgical masks lowered
the number of aerosol droplets behind the mask still by a
substantial 4-fold compared to outside of the mask. It is plausible
that for larger spray droplets from cough expulsions the difference
between surgical masks and the F95 respirator masks would be even
smaller. Interestingly, for outward protection, the effectiveness
and differences are much smaller (see numbers in the FIG. 5).
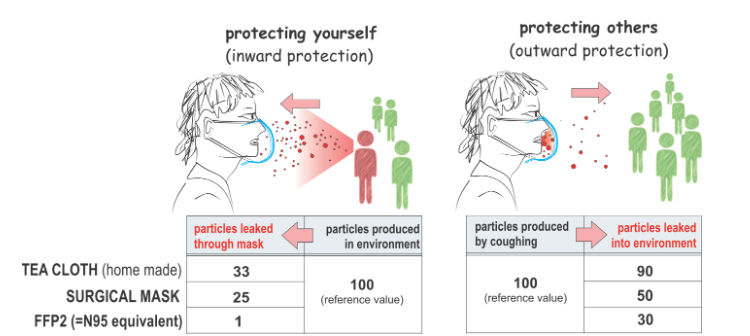
FIGURE 5. Filtering effect for small droplets (aerosols) by various masks; home-made of tea cloth, surgical mask (3M “Tie-on”) and a FFP2 (N95) respirator mask. The numbers are scaled to the reference of 100 (source of droplets) for illustrative purposes, calculated from the PF (protection factor) values in Table 2 of van der Sande et al, 2007. Measurement was performed with a Portacount counter that registers particles in the air with sizes in the range between 0.02 and 1 micrometer at the end of a 3-hour wearing period with no physical activity. The number for the protection are medians of 7 (or 8) adult volunteers per group. Protection at the beginning of the test was similar for the Tea Cloth and Surgical mask, but for FFP2 the protection was double. Children experienced substantially less protection (see van der Sande et al 2007)
These results raise the urgent question: If all we want is to mitigate the pandemic, that is, to “flatten the curve”, how much does a 4-fold reduction of particles that reach the lungs decrease transmission from person to person? Intuition suggests that even an imperfect mask may offer some protection that is at least in the range of the recommended separation by more than 6 feet in social interactions or wasing hands or not touching your face — all recommendation based on mechanistic plausibility without strong epidemiological support.
Technically, one could quantify by how much the reduction by 4-fold
of the droplets that a person is exposed to, as achieved by surgical
masks, or by 3-fold, as achieved by makeshift tea-cloth masks,
contributes to a reduction of the “reproduction rate” from the
initial R0 to the effective Rt after mitigation intervention at
time t. Perhaps by 25%? Then one could, using
But such “bottom up” calculation of R is complicated because it would require knowledge of many mechanistic factors that are not easy to quantify. For instance, we do not know to what proportion COVID-19 is transmitted via large spray droplets vs. small aerosols. Only in the latter case will the advantage of N95 respirator masks over surgical masks be fully realized! We also do not know how much social distancing alone contributes to reducing R.
Thus, let us have a look at the actual biology of transmission which offers a way out of this problem and has also not been considered by officials who claimed that “surgical masks are not effective”.
III. THE BIOLOGY
The SARS-Cov-2 virus, like any virus, must dock onto human cells using a key-lock principle, in which the virus presents the key and the cell the lock that is complementary to the key to enter the cell and replicate. For the SARS-Cov-2 virus, the viral surface protein “Spike protein S” is the “key” and it must fit snugly into the “lock” protein that is expressed (=molecularly presented) on the surface of the host cells. The cellular lock protein that the SARS-Cov-2 virus uses is the ACE2 protein FIG 6).
This cell surface enzyme normally has a cardio-pulmonal protective function. ACE2 is expressed at higher levels in the elderly, in people with chronic heart failure or with pulmonary or systemic arterial hypertension. (Note that ACE2 expression is “rate –limiting” because other host proteins whose presence is also needed for the virus to enter the cells, such as proteases, are more abundantly and widely expressed). Certain blood pressure drugs (as now intensely discussed since hypertension is a risk factor for progression to ARDS and death in COVID-19), but also mechanical stress from ventilation, ironically, can increase the expression of ACE2.
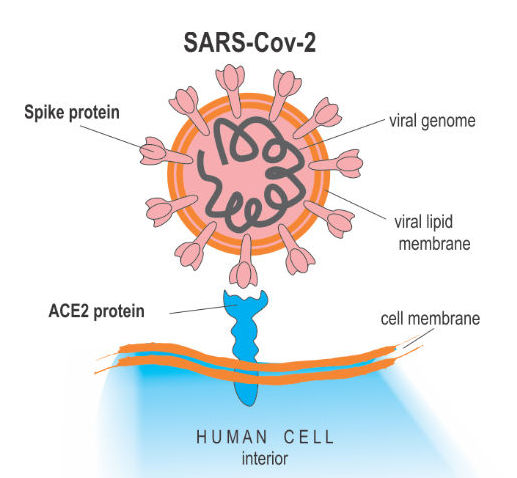
Figure 6. The SARS-Cov-2 enters the host cell by docking with its Spike protein to the ACE2 (blue) protein in cell surfaces.
Surprisingly, ACE2 expression in the lung is very low: it is limited to a few molecules per cell in the alveolar cells (AT2 cells) deep in the lung. But a just published paper by the Human Cell Atlas (HCA) consortium reports that ACE2 is highly expressed in some type of (secretory) cells of the inner nose! (FIG. 7).
Combine this fact with the above explanation of the mechanics: The nasal expression of ACE2 protein suggests that the SARS-Cov2 virus infects these cells. One can also infer that transmission of the SARS-Cov2 virus will occur largely via large cough or sneeze droplets, which comprise the vast portion of the sprayed liquid in cough/sneeze and will land in the nasopharynx due to their size — precisely where the molecular locks for the virus are present, allowing viral attachment and entry into the host cells. Obviously this route of transmission could be effectively blocked by simple physical barrier. (The proximal expression of ACE in the nasal cavity also supports the transmission by surface droplets — hence, indeed wash your hands).
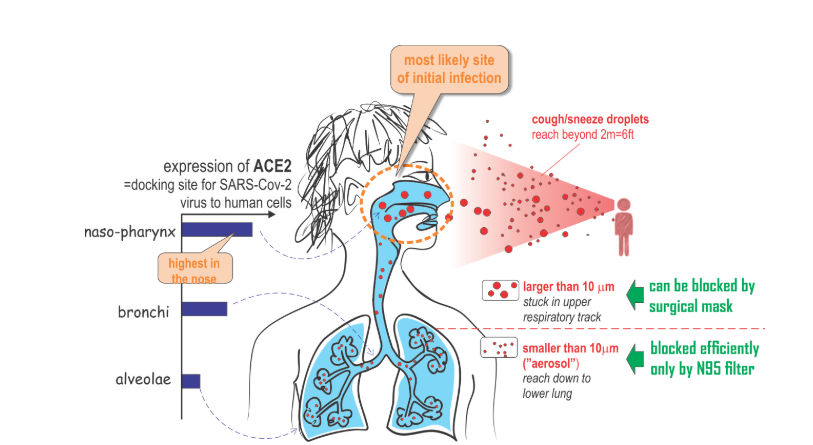
FIGURE 7. Major route of viral entry is likely via large droplets that land in the nose — where expression of the viral entry receptor, ACE2 is highest. This is the transmission route that could be effectively blocked already by simple masks that provide a physical barrier.
In fact, Wölfel et al. now report that viral material can be readily detected and isolated from nasal swabs, unlike in the case of other airborne viral infections, such as the original SARS. Compared to SARS (which also uses ACE2 to enter cells) in the case of COVID-19, viral genomes (RNA) appear earlier in nasal swabs and at much higher concentration, such that detection is rather easy. In fact, the FDA just approved swabs for tests taken from just from the front of the nose through self-collection, instead of deep in the nasopharynx. The molecular analysis also show that the SARS-Cov2 virus is active and replicates already in the nasopharynx, unlike other respiratory viruses that dwell in deeper regions of the lung.
The viral replication in the nasopharygeal mucosa may also explain
positive tests in the prodromal stage and transmission by healthy
carriers, and perhaps the
From a practical and societal point of view, surgical or self-made masks, if handled properly, will at worst not hurt and may at best, help. (Make sure to discard or launder after use without touching the outward surface). These simpler, inexpensive masks may suffice to help to flatten the curve, perhaps a bit, perhaps substantially. Importantly: using them will not take away valuable N95 respirator masks from health care workers.
THE IMPLICATIONS
It would be tragic if the wrong logics and mechanics and biology, which has led Western governments to not encourage, if not stigmatize the wearing of masks, may have contributed to the steep rise of COVID-19. Given that the upper respiratory tract is the major site for SARS-Cov-2 entry into human tissues, wearing simple face masks which exert a barrier function that blocks those big projectile droplets that land in the nose or throat may substantially reduce the production rate R, to an extent that may be comparable to social distancing and washing hands. This would then double the effect of mitigation in “flattening the curve”!
Looking forward: if we are soon loosening the
lockdown due to the political pressure to sustain the economy,
perhaps encouraging face masks to be worn in the public would be a
good compromise between total lockdown and total freedom that risks
resurgence of the invisible enemy. There is now a robust scientific
basis for putting an end to the officials’ anti-surgical mask
hysteria and to recommend or even mandate a broad use of masks as in
Asian countries that have bent the curve.
PS (April 1, 2020): T
Stay up to date on coronavirus (Covid-19)
Follow the Medium Coronavirus Blog or sign
up for the newsletter to read
expert-backed coronavirus stories from Medium and across the web,
such as :
.